The Importance of Organ Donation: A Family’s Story
From 1998 to today, India has witnessed an increase in paediatric liver transplant surgeries. The country’s requirement for these procedures is estimated at 2500-3000 annually, but less than 200 are carried out yearly.
*Ankit(name changed to protect privacy) from Vikhroli, Mumbai, looks like a typical young IT employee. He has a cheerful demeanour and lives happily with his 2-year-old son *Dhruv(name changed to protect privacy) and his wife. However, a few months ago, it was a different story for the family.
Nibish was diagnosed with a rare genetic disorder called Progressive Familial Intrahepatic Cholestasis (PFIC-2) and had jaundice immediately after birth.
PFIC-2 is a rare condition that affects one in 50,000-1,00,000 newborns worldwide. According to www.hopkinsmedicine.org, “Progressive familial intrahepatic cholestasis (PFIC) is a disorder that causes progressive liver disease, typically leading to liver failure. In people with PFIC, liver cells are less able to secrete bile, and the buildup of bile in liver cells causes liver disease.” The only treatment is liver transplant surgery. The paediatric liver transplant requirement is 1 to 2 per million population (worldwide).
In the last year, Nibish was admitted to a hospital four times in very critical condition, every time requiring ICU care. When the boy was two years old, doctors informed the middle-class family that he would require a liver transplant. Nibhish’s mother wanted to donate a part of her liver, but she was diagnosed with uncontrolled diabetes and was started on treatment and a strict dietary regime.
Liver transplantation is a well-established treatment for children with End-Stage-Liver-Disease (ESLD). It is estimated that India needs 4000 liver transplants annually, but we are nowhere near meeting this demand. A multitude of reasons account for the large disparity between demand and supply. Surgical expertise, financial constraints, and donor shortages are the main reasons. Even though the cost is cheaper than in western countries, it’s still a financial burden for Indian families.
Dr Pradnya Bendre, Head of Pediatric Surgery at Bai Jerbai Wadia Hospital, notes that because the mother had diabetes, the father was asked to consider donating. It was not an easy decision for the family, as they struggled to make ends meet being a middle-class family with compounding medical bills. Still, Ankit ran around to earn and raise the funds and to make this work for his family.
Courage and Resilience
Yogesh underwent a physical evaluation and was told he was very overweight. Doctors put him on a strict diet plan which included a lot of protein and leafy vegetables. “I joined a gym and lost ten kilos for the surgery, and I worked out two hours daily to attain the ideal weight,” adds Ankit.
Meanwhile, he also tried to find out how much the surgery would cost and realised it was around Rs 24-27 lakhs in private hospitals.
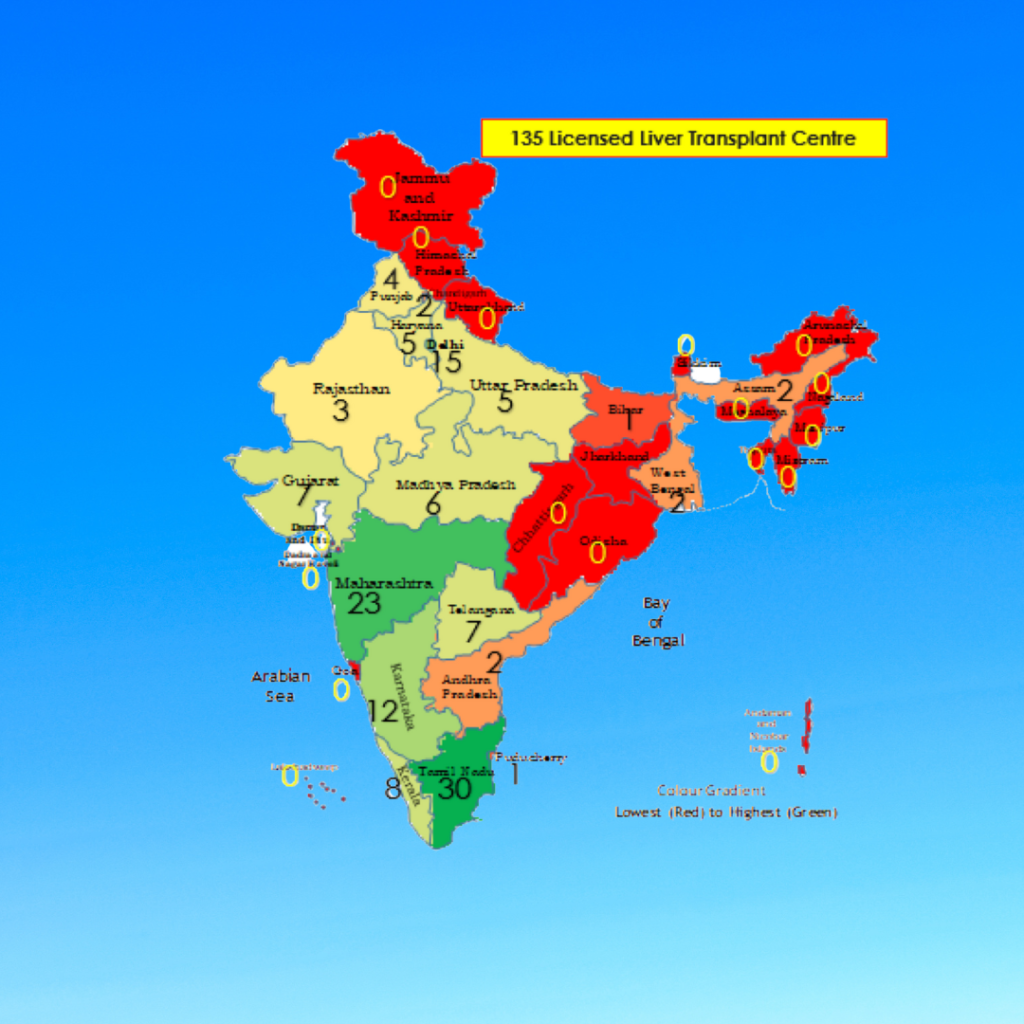
Source: https://www.indianpediatrics.net/dec2020/1110.pdf
On October 16, 2022, *Dhruv underwent a living donor liver transplant at Bai Jerbai Wadia Hospital, a charity hospital. The surgery took 7 hours for the donor and 8 hours for the recipient.
However, recovery was not so easy for the child. He was on a ventilator and required rigorous chest physiotherapy 4-5 times daily, and NasoGastric feeds. His total ICU stay was 28 days. Today, he is off oxygen, stable, eating by himself, getting up, trying to stand and can talk with his parents.
The surgery was conducted by a team of doctors from Wadia who were mentored by Darius Mirza, the Chief Transplant Surgeon from Birmingham Children’s Hospital, UK. He notes that liver transplantation is the best option for a patient diagnosed with end-stage liver disease. Not only adults but even a large number of children are waiting for a liver transplant. Organ donation can save lives. Pledge to donate them and help needy patients,” he adds.
When it comes to live donor transplantation, it is mainly the parents who are required to part with a portion of their liver to save the child’s life at personal risk. This is an added burden for families already coping with a child’s illness and medical costs. While the parents’ sacrifice is noble, it does beg the question – why are we not promoting and developing a more robust deceased donor network?
One of the oldest medical institutes in the city shows the way
Bai Jerbai Wadia Hospital, a public-private partnership hospital, is a teaching hospital with 525 beds, and over 60 paediatrics specialists, catering to more than 150,000 children on an outpatient basis and approximately 10,000 children as inpatients annually. With 155 beds, Bai Jerbai Wadia Hospital has one of the world’s largest Neonatal Intensive Care Units (NICU).BMC bears 75% of the operational cost of the hospital, according to news reports.
“Wadia hospital caters to 3-5 prospective liver transplant patients monthly. But most of these are nuclear families with limited family support, young parents who have just started earning and don’t have adequate health insurance coverage. Along with that, there is the need for repeated hospital admissions and lifelong medication after transplantation which act as major deterrents when a family has to decide for the child to have a transplant,” says Dr Minnie Bodhanwala, CEO of Wadia Hospitals.
The hospital has showcased a way of improving access to a life-saving procedure for the indigent by providing financial support for the families from local authorities, charity organisations and even crowd-funding.
India has made great strides in organ transplantation in recent years. However, the rate of transplants is still low when compared to other countries. There are many reasons for this, but one of the most important is that people do not know enough about organ donation and transplantation. More needs to be done to promote organ donation and transplantation in India. This includes increasing awareness among the population, training more surgeons, and developing better infrastructure. With concerted effort, we can increase the number of successful organ transplants in India and improve the quality of life for thousands of patients waiting for a donor organ.




